
Background:
Retroperitoneal schwannoma is a rare tumor rising from Schwann cells in peripheral nerve sheaths. Retroperitoneal schwannoma is really infrequent and has nonspecific symptoms and imperfect radiologic features, and is often identified histologically after surgery.
Case Report:
We report the case of a 73-year-old man presented with flank mass. Imaging shows a hypoechoic macro lobulated solid cystic mass in retroperitoneum. Intraoperatively, after complete resection of retroperitoneal mass, a suspected lesion in upper pole of right kidney was observed. Histopathology evaluation after surgery shows coexistence of a large retroperitoneal schwannoma and papillary renal cell carcinoma, type 1.
Conclusion:
Schwannoma should be considered in the differential diagnosis of retroperitoneal spindle cell tumor. Schwannoma coexisted with renal cell carcinoma in a patient is an unusual event. Thus, it can show the importance of appropriate evaluation before any surgery.
Keywords:
Renal cell carcinoma, Retroperitoneum, Schwannoma
Department of pathology, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran
Tel:/Fax: +98 21 6634 8580
Email: elhamnazar@yahoo.com
Received: Feb 5 2022
Accepted: May 24 2022
Citation to this article:
Moradi Tabriz H, Nazar E, Sharbati F, Rezaei Z. Synchronous Retroperitoneal Schwannoma and Incidental Papillary Renal Cell Carcinoma: A Case Report. J Iran Med Counc. 2023;6(1):174-78.
Schwannoma is a benign tumor originating from Schwann cells. The most common places for schwannoma are head, neck and extremities, and it can arise in retroperitoneal area (1). Almost 0.3% to 3.0% are originate in the retroperitoneum, accounting for 0.5-1.2% of all retroperitoneal tumors (2). Histologically, some schwannoma variants have been described: common, plexiform, cellular, epithelioid, and ancient (3). Also, schwannoma with cystic degeneration such as calcification and xanthomatous infiltration are explained (4). The precise diagnosis of retroperitoneal schwannoma before surgery is problematic. Imaging modalities have confident diagnostic worth but absence specificity (5). Also, coexistence of schwannoma and other malignancies are infrequent. Here, we present an extremely rare case of the combination of a synchronous papillary renal cell carcinoma, type 1 and schwannoma in a 73-year-old male.
A 73-year-old man with history of a flank mass from 4 years ago who presented with progressive flank pain from 20 days ago was referred to the department of urology of Sina hospital affiliated with the Tehran University of Medical Sciences. The first outpatient examination findings were unremarkable. The patient’s medical and family histories were unremarkable. Laboratory data was in a normal range. On imaging, ultrasonography revealed a hypo-echoic macro lobulated mass M: 100×96×92 mm in the right retroperitoneal area. Magnetic Resonance Imaging (MRI) showed right retroperitoneal mass with hemorrhage and calcification on T1, multiple cystic components on T2 and thick peripheral enhancement on post contrast images which have been compared with 4 years ago imaging and showed no change in size and manner (Figure 1). Based on clinicoradiologic findings, the patient underwent surgery. Intraoperatively, a cystic encapsulated mass was found in the right retroperitoneal. The mass had no adhesion to the liver or major vessels and was completely removed. Also, intraoperation gross examination of the right kidney revealed a suspicious lesion the in upper
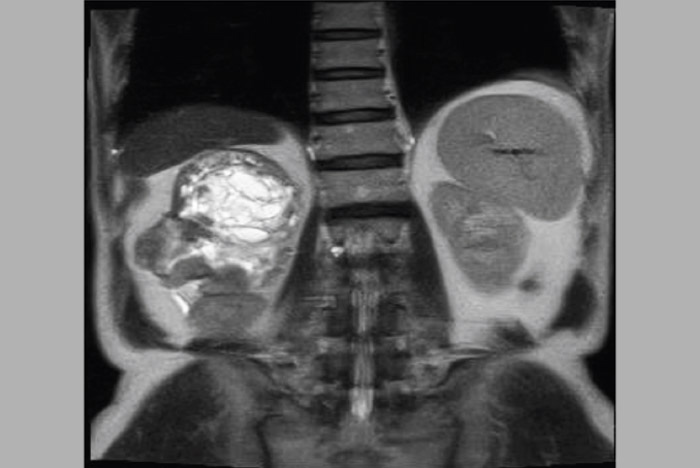
Figure 1. Magnetic resonance imaging showed right retro- peritoneal mass with hemorrhage and calcification.

Figure 2. Gross examination of retroperitoneal mass showed cystic lobulated mass.
surgery, the specimen was sent for histopathologic examination. On macroscopic examination, a well- defined encapsulated tan lesion with lobulation and calcification was observed. On cut sections revealed a tan heterogeneous surface with hemorrhage and calcification (Figure 2). Microscopic examination revealed a biphasic spindle cell tumor, composed of hyper cellular and hypo cellular areas (Antoni A and Antoni B) with large irregular spaced vessels, the tumor cells were narrow with taper ends, dense chromatin and have been arranged in fascicles.
changes like calcification and xanthomatous changes were observed. The tumor was positive for S100 on Immunohistochemistry (IHC) staining and established schwannoma (Figure 3). Second specimen from right kidney mass composed of a papillary architecture with fibrovascular cores, infiltrated by neutrophils and
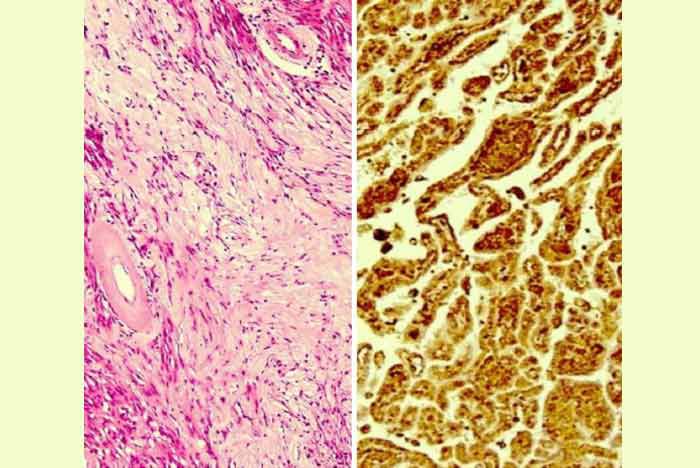
Figure 3. Histopathologic and immunohistochemistry ex- amination showed Schwannoma with spindle cells arranged (left) and positive S100 (right) staining.
foamy macrophages. IHC staining showed positive staining for CD10, vimentin, and Cytokeratin 7. Therefore, according to the histopathologic and IHC findings, papillary renal cell carcinoma, type 1 was confirmed (Figure 4).
Schwannomas originate from Schwann cells which proliferate and dislocate the normal components of the nervous tissue (6). Retroperitoneal schwannoma is really infrequent and have broad-spectrum symptoms and restricted radiologic findings, and need diagnose histologically after surgical resection (7). About 5-8% cases of schwannoma are in relationship with Von Recklinghausen’s disease. Retroperitoneal schwannoma is more usually re- cognized in paravertebral spaces or presacral area. Retroperitoneum is uncommon location in absence of Von Recklinghausen’s disease for schwannoma (8). Papillary renal cell carcinoma is about 15 to 20% of renal cell carcinomas and is a heterogeneous carcinoma with various types of phenotype including indolent or aggressive behavior (9). Schwannomas
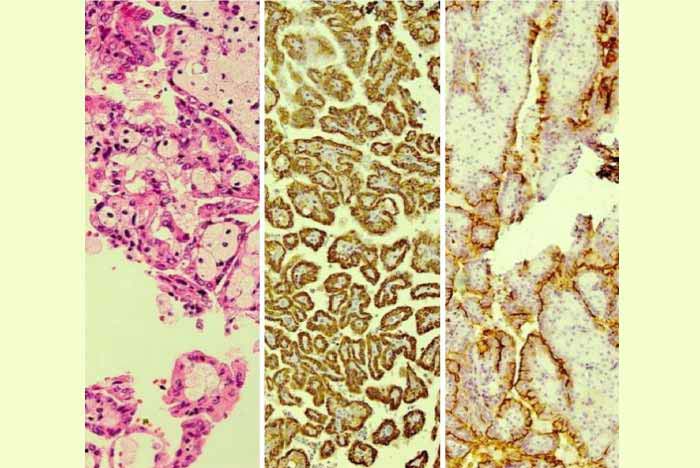
Figure 4. Histopathologic and immunohistochemistry examination showed papillary architecture with fibrovascular cores, infiltrated by neutrophils and foamy macrophages (left), positive Cytokeratin 7 (middle), and positive CD10 (right) staining.
are problematic to establish preoperatively from radiology features. In 1989, Ghiatas and Faleski explained the computed tomography findings of a benign schwannoma as a well-defined homogeneous or nonhomogeneous soft mass (10). But there are no pathognomonic findings on imaging assessment. Preoperative biopsy is not suggested for complication risks; however, for diagnosis and treatment, surgery is obligatory (11). In schwannomatosis, germline SMARCB1 or LZTR1 mutations prompt to the expansion of numerous benign schwannomas. Also, other tumors may happen in patients with schwannomatosis (12). Genetic studies were not usually available in synchronous tumors. In our case, other sites with schwannoma cannot be found but synchronous tumor such as papillary renal cell carcinoma, type 1 was discovered which maybe import germline mutations. Acknowledgment and alertness of these rare, benign schwannoma will notice in the differential diagnosis of spindle cell tumors of retroperitoneum and avoid their misinterpreted as invasive sarcomatoid renal cell carcinomas or other sarcomas (13). The most vital difference is with invasive sarcomatoid renal cell carcinoma. While renal cell carcinoma may have widespread extents with a spindle pattern, watchful examination should expose foci of more typical carcinoma appearance. Also, sarcomatoid renal cell carcinoma is invasive with infiltrative growth pattern and does not display the well-bordered capsule observed in all of cases of schwannoma. Histologically, Schwannoma consists of spindle-shaped tumor cells with the Antoni A (hyper cellular) and Antoni B (hypocellular) areas. IHC staining for S100 are almost generally positive in these tumors (14). Qiang Li et al in retrospective analysis of 84 patients between 1951 and 2004 showed only 2 retroperitoneal schwannoma co-occurrences with other malignancies (colon adenocarcinoma and squamous cell carcinoma of lung), but genetic studies were not done (15). Our case is a unique case of a
benign retroperitoneal schwannoma that have been accompanied by papillary renal cell carcinoma, type
1. This case is of attention for both its infrequency and its uncommon coexistence. Whether or not such a concurrence is a simple incidental association or the two lesions are associated with an underlying connection require supplementary study. According to the really low incidence rate of the papillary renal cell carcinoma and schwannomas, we presume that the concomitant is accidental. Inclusive, we reported an exceptional rare case of synchronous existence of retroperitoneal schwannoma, accompanied by renal cell carcinoma of the kidney, which has not been informed in the literature. We recommend genetic studies to recognize same molecular pathway in synchronous tumors.
Schwannoma must be noticed in the differential diagnosis of spindle cell tumors of the retroperitoneum. Spindle cells of schwannoma in this site may be due to misdiagnosis of the quite more usually happening invasive sarcomatoid renal cell carcinoma. Schwannoma coexisted with renal cell carcinoma in a patient is an uncommon incident. Thus, it can show the importance of appropriate imaging and assessment before any surgery.
None.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
None.
Copyright © 1400 All material and intellectual rights to the site belong to the Farjad Group.